A cyst is a benign, round, dome-shaped encapsulated lesion that contains fluid or semi-fluid material. It may be firm or fluctuant and often distends the overlying skin. They’re usually benign but may need treatment for complications.

A cyst is a sac-like pocket of membranous tissue that contains fluid, air, or other substances. Cysts can grow almost anywhere in your body or under your skin. Cysts are different from abscesses, which are collections of pus from an infection.
Cysts are very common, affecting at least 20% of adults. They may be present at birth or appear later in life. They arise in all races. Most types of cysts are more common in males than in females.
There are hundreds of different types of cysts. These form in different parts of your body. Whether a cyst needs treatment depends on a number of factors, including:
- the type of cyst
- the location of the cyst
- whether the cyst is causing pain or discomfort
- whether the cyst is inflamed or infected
- Some of the common types are:
- Baker’s cyst — behind your knee
- Bartholin’s cysts — on your vulva
- Breast cysts
- Acne epidermoid cysts and sebaceous cysts —on your skin
- Ganglion cysts — in your wrists, fingers or feet
- Kidney cysts
- Ovarian cysts
Epidermoid cysts are due to the proliferation of epidermal cells within the dermis. Their origin is the follicular infundibulum. Multiple epidermoid cysts may indicate Gardner syndrome. The common term, sebaceous cyst, is a misnomer.


An epidermal inclusion cyst is a response to an injury. Skin is tucked in to form a sac that is lined by healthy epidermal cells that continue to multiply, mature and form keratin.
Epidermoid cysts occur on face, neck, trunk or anywhere where there is little hair.
Most epidermoid cysts arise in adult life.
They are more than twice as common in men as in women.
They present as one or more flesh–colored to yellowish, adherent, firm, round nodules of variable size.
A central pore or punctum may be present.
An epidermoid cyst is also called a follicular infundibular cyst, epidermal cyst, and keratin cyst.
Trichilemmal cyst


90% of trichilemmal cysts occur on the scalp; otherwise face, neck, trunk, and extremities.
Most trichilemmal cysts arise in middle age.
In 70% of cases, trichilemmal cysts are multiple.
They present as adherent, round or oval, firm nodules.
There is no punctum.
The keratinous content is firm, white and easily enucleated.
A trichilemmal cyst is also called pilar cyst.
Steatocystoma

A solitary steatocystoma is known as steatocystoma simplex.
More often, there are multiple lesions (steatocystoma multiplex) on the chest, upper arms, axillae, neck and scrotum or vulva.
The cysts arise in the late teens and 20s due to the effect of androgens and persist lifelong.
They are freely moveable, smooth flesh to yellow color papules 3–30 mm in diameter.
There is no central punctum.
Content of cyst is predominantly sebum.
Dermoid cyst

A cutaneous dermoid cyst may include skin, skin structures and sometimes teeth, cartilage and bone.
Most dermoid cysts are found on face, neck, scalp; often around eyelid, forehead and brow.
It is a thin-walled tumor that ranges from soft to hard in consistency.
The cyst is formed at birth, but may not present until an adult.
Ganglion cyst


A ganglion cyst most often involves the scapholunate joint of the dorsal wrist.
These arise in young to middle-aged adults.
They are three times more common in women than in men.
The cyst is a unilocular or multilocular firm swelling 2–4 cm in diameter that transilluminates.
Cyst contents are mainly hyaluronic acid, a golden-colored goo.
Hidrocystoma

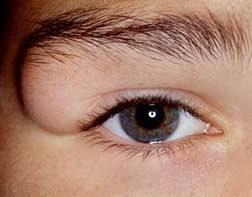
Hidrocystoma is a translucent jelly-like cyst arising on an eyelid.
It is also known as cystadenoma, Moll gland cyst, and sudoriferous cyst.
The common solitary translucent eyelid cyst is an apocrine hidrocystoma.
Multiple cysts on the lower eyelid are eccrine hidrocystomas.
Pilonidal cyst

A pilonidal cyst is a common skin condition that forms in the cleft at the top of your buttocks. It consists of a small hole or tunnel in the skin that may become infected and fill with fluid or pus and it typically occurs Trusted Source after puberty.
Changing hormones, hair growth, and friction from clothes or from spending a long time sitting may all cause a pilonidal cyst.
Symptoms of an infection include:
pain when sitting or standing, discolored or sore skin around the area, pus or blood draining from the abscess, causing a foul odor, swelling of the cyst, hair protruding from the lesion
Mucous cyst

A mucous cyst is a fluid-filled lump that forms on your lip or around your mouth when the salivary glands become plugged with mucus. The most common causes of mucous cysts include:
Lip or cheek biting
Lip piercings
Rupture of the salivary gland
Improper dental hygiene
Mucous cysts will often go away on their own. But if you have recurring or frequent mucous cysts, you may need medical treatment.
Digital myxoid pseudocyst

Mucous/myxoid pseudocysts arise in older adults on the distal phalanx
They arise from distal interphalangeal joint, associated with osteoarthritis.
They often present as a longitudinal depression in the nail due to compression on the proximal matrix.
Vulval mucous cyst:

Vulvar mucinous cysts are rare, benign, noninvasive masses. They can be mistaken for cysts of Bartholin gland, Skene gland, vestibular, or canal of Nuck.
It presents as a soft swelling in the introitus of the vagina: a posterior swelling is a Bartholin cyst and a periurethral swelling is a Skene cyst.
Generally, they may be left untreated, but observed. However, if symptomatic, they may require surgical removal.
Baker’s cyst: A Baker’s cyst is a fluid-filled sac that forms in the popliteal fossa, which is located on the posterior aspect of the knee. In adults, Baker’s cysts are commonly associated with degenerative conditions of the knee, and patients may present with tightness, discomfort, or pain behind the knee.


Baker’s cysts are encountered most frequently in adults with a history of trauma (e.g., cartilage or meniscus tears, injury to the knee), in association with degenerative/co-existing knee joint disease (e.g., osteoarthritis, rheumatoid arthritis, infectious arthritis, meniscal tears), or asymptomatically as an incidental finding.
Baker’s cysts form and can expand as a result of the accumulation and extrusion of synovial fluid that localizes between the semimembranosus and medial head of the gastrocnemius. In some instances, normal anatomic variants entail physiologic capsular openings or defects in the posterior knee joint capsule that is essentially contiguous with the gastrocnemius-semimembranosus bursa. Popliteal cysts are located on the medial side of the popliteal fossa just below the crease found at the posterior knee.
Treatment is not usually necessary for a Baker’s Cyst unless the patient is symptomatic.
Incidental findings in the asymptomatic patient are managed with observation and reassurance alone.
Non-operative management:
- Rest/activity modification
- NSAIDs
- PT/rehab regimens are often effective in patients with minimal symptoms and in the setting of smaller degenerative meniscal tears
- Aspiration and steroid injection
- The knee joint itself can be treated with a cortisone injection in the setting of moderate to advanced tricompartmental degenerative knee arthritic conditions. This can help manage patients’ symptoms and clinically differentiate the contribution of the popliteal cyst itself on the patient’s daily symptoms
- Ultrasound-guided aspiration and injection can be performed by an experienced interventional radiologist
- Recurrence rates are much lower in younger patient populations
- Recurrence rates are higher in older patient populations and degenerative meniscal tears with associated cysts
- Operative management
- Arthroscopic debridement, cyst decompression, meniscal repair vs partial meniscectomy
- Open cyst excision
Kidney cyst: Kidney cysts are round pouches of fluid that form on or in the kidneys. Kidney cysts can occur with disorders that may impair kidney function. But more often, kidney cysts are a type called simple kidney cysts. Simple kidney cysts aren’t cancer and rarely cause problems.
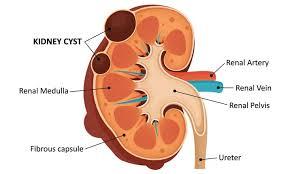
Simple kidney cysts aren’t the same as cysts that form with polycystic kidney disease. Simple cysts also differ from complex cysts. Complex cysts need to be watched for changes that could be cancer.
Simple kidney cysts typically don’t cause symptoms. But if a simple kidney cyst grows large enough, symptoms may include:
Dull pain in the back or side
Fever
Upper stomach pain
Kidney cysts may sometimes lead to complications, including:
An infected cyst. A kidney cyst may become infected, causing fever and pain.
A burst cyst. A kidney cyst that bursts causes severe pain in the back or side. Sometimes a burst cyst may cause blood in the urine.
Blocked urine flow. A kidney cyst that blocks the typical flow of urine may lead to kidney swelling.
Ovarian cyst:
Ovarian cysts are fluid-filled sacs in the ovary. They are common and usually form during ovulation. Ovulation happens when the ovary releases an egg each month. Many women with ovarian cysts don’t have symptoms. The cysts are usually harmless.
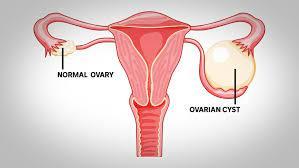
The two most common types of cysts are:
Follicle cysts: In a normal menstrual cycle, an ovary releases an egg each month. The egg grows inside a tiny sac called a follicle. When the egg matures, the follicle breaks open to release the egg. Follicle cysts form when the follicle doesn’t break open to release the egg. This causes the follicle to continue growing into a cyst. Follicle cysts often have no symptoms and go away in one to three months.
Corpus luteum cysts: Once the follicle breaks open and releases the egg, the empty follicle sac shrinks into a mass of cells called corpus luteum. Corpus luteum makes hormones to prepare for the next egg for the next menstrual cycle. Corpus luteum cysts form if the sac doesn’t shrink. Instead, the sac reseals itself after the egg is released, and then fluid builds up inside. Most corpus luteum cysts go away after a few weeks. But, they can grow to almost four inches wide. They also may bleed or twist the ovary and cause pain. Some medicines used to cause ovulation can raise the risk of getting these cysts.
Other types of benign ovarian cysts are less common:
- Endometriomas are caused by endometriosis. Endometriosis happens when the lining of the uterus (womb) grows outside of the uterus.
- Dermoids come from cells present from birth and do not usually cause symptoms.
- Cystadenomas are filled with watery fluid and can sometimes grow large.
In some women, the ovaries make many small cysts. This is called polycystic ovary syndrome (PCOS). PCOS can cause problems with the ovaries and with getting pregnant.
Malignant (cancerous) cysts are rare. They are more common in older women. Cancerous cysts are ovarian cancer. For this reason, ovarian cysts should be checked by your doctor. Most ovarian cysts are not cancerous.
Most ovarian cysts are small and don’t cause symptoms.
If a cyst does cause symptoms, you may have pressure, bloating, swelling, or pain in the lower abdomen on the side of the cyst. This pain may be sharp or dull and may come and go.
If a cyst ruptures, it can cause sudden, severe pain.
If a cyst causes twisting of an ovary, you may have pain along with nausea and vomiting.
Less common symptoms include:
- Pelvic pain
- Dull ache in the lower back and thighs
- Problems emptying the bladder or bowel completely
- Pain during sex
- Unexplained weight gain
- Pain during your period
- Unusual (not normal) vaginal bleeding
- Breast tenderness
- Needing to urinate more often
Complications of cysts
- Rupture of a cyst
- The contents of the cyst may penetrate the capsular wall and irritate the surrounding skin.
- The area of tender, firm inflammation spreads beyond the encapsulated cyst.
- Sterile pus may be discharged.
- Secondary infection
- A ruptured cyst may infrequently become secondarily infected by Staphylococcus aureus, forming a furuncle (boil).
- Pressure effect
- A dermoid cyst can cause pressure on underlying bony tissue.
- A ganglion cyst can cause joint instability, weakness, limitation of motion and may compress a nerve.
- A digital mucous cyst may place pressure on the proximal matrix and cause a malformation of the nail.
- Malignancy
- Cutaneous cysts and pseudocysts are non-proliferative benign lesions.
Nodulocystic basal cell carcinoma is a common skin cancer that presents as a rounded nodule and may initially be mistaken for a cyst, but steady enlargement, destruction of the epidermis with ulceration and bleeding occur eventually.
A malignant proliferative trichilemmal cyst is a misnomer. It is an extremely rare tumor.
How are cysts diagnosed?
Cysts have typical clinical characteristics. When a cyst is surgically removed, it should undergo a histological examination. The type of lining of the wall of the cyst and the cyst contents help the pathologist classify it.
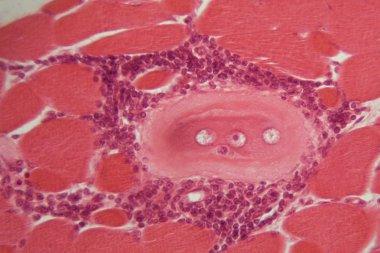
An epidermoid cyst is lined with stratified squamous epithelium that contains a granular layer. Laminated keratin contents are noted inside the cyst. An inflammatory response may be present in cysts that have ruptured.
Trichilemmal cysts have a palisaded outer layer without a granular layer. The contents are eosinophilic hair keratin. Older cysts may exhibit calcification. The proliferating variety is considered a tumor.
Steatocystoma has a folded cyst wall with prominent sebaceous gland lobules.
A dermoid cyst contains fully mature elements of the skin including fat, hairs, sebaceous glands, eccrine glands, and in 20%, apocrine glands.
The lining of the wall of a ganglion cyst or digital mucous cyst is collagen and fibrocytes. It contains hyaline material.
Hidrocystoma has a thin lining wall of eosinophilic bilaminar cells.
What is the treatment for cysts?
An asymptomatic epidermoid cyst does not need to be treated. In most cases, an attempt to remove only the contents of a cyst is followed by recurrence. If desired, cysts may be entirely excised. Recurrence is not uncommon, and re-excision may be surgically challenging.
Inflamed cysts are sometimes treated with:
- Incision and drainage
- Intralesional injection with triamcinolone
- Oral antibiotics
- Delayed excision biopsy


