Skin cancer is the out-of-control growth of abnormal cells in the epidermis, the outermost skin layer, caused by unrepaired DNA damage that triggers mutations. These mutations lead the skin cells to multiply rapidly and form malignant tumors.

Skin cancers can look quite different from one person to another due to skin tone, size and type of skin cancer and location on the body. Skin cancer develops primarily on areas of sun-exposed skin, including the scalp, face, lips, ears, neck, chest, arms and hands, and on the legs in women. But it can also form on areas that rarely see the light of day — your palms, beneath your fingernails or toenails, and your genital area.


The two main causes of skin cancer are the sun’s harmful ultraviolet (UV) rays and using UV tanning beds.
Other risks include:
- Smoking (especially for SCC)
- Human papillomavirus infection (genital warts), particularly for mucosal sites such as oral mucosa, lips, and genitals
- Drug-induced immune suppression, for example in patients who have received an organ transplant and are on azathioprine and ciclosporin
- Other medicines such as hydrochlorothiazide
- Human immunodeficiency virus infection (HIV)
- Exposure to ionizing radiation
- Exposure to certain chemicals, such as arsenic and coal tar
- Longstanding skin diseases such as lichen sclerosis, lupus erythematosus, linear porokeratosis or cutaneous tuberculosis
- A longstanding wound or scar, for example, from a thermal burn.
The good news is that if skin cancer is caught early, your dermatologist can treat it with little or no scarring and high odds of eliminating it entirely. Often, the doctor may even detect the growth at a precancerous stage, before it has become a full-blown skin cancer or penetrated below the surface of the skin.
Skin cancer most commonly affects older adults, but it can also affect younger adults, and rarely, children.
Skin cancer tends to affect individuals with fair skin (Fitzpatrick skin phototype I, II and III), although people with darker skin can also develop skin cancer.
People who have had skin cancer have an increased risk of developing other skin cancers.
A family history of skin cancer also increases risk.
Certain genes such as melanocortin-1 receptor have been identified as carrying an increased risk of skin cancer.
Some skin cancers are due to genetic conditions, such as:
- Albinism
- Basal cell naevus syndrome (Gorlin syndrome)
- Bazex–Dupré–Christol syndrome
- Bloom syndrome
- Brooke-Spiegler syndrome
- Cowden disease
- Dyskeratosis congenita
- Epidermolysis bullosa
- Epidermodysplasia verruciformis
- Familial atypical multiple mole and melanoma syndrome (FAMMM)
- Premature aging syndromes (progeria)
- Rothmund-Thomson syndrome
- Muir-Torre syndrome
- Xeroderma pigmentosum.
Signs of advanced, aggressive, or neglected skin cancer may include:
- Ulceration
- Bleeding
- Local invasion and destruction of adjacent tissues and structures
- Distant spread of a tumor to lymph glands and other organs such as liver and brain (metastasis).
The main types of skin cancer are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), melanoma and Merkel cell carcinoma (MCC).
The term non-melanoma skin cancer refers to all types of skin cancer apart from melanoma. BCC and SCC are also called keratinocyte cancer.
Basal cell carcinoma:
Basal cell carcinoma is a type of skin cancer. Basal cell carcinoma begins in the basal cells — a type of cell within the skin that produces new skin cells as old ones die off. Basal cell carcinoma often appears as a slightly transparent bump on the skin, though it can take other forms. It may appear as a pearly or waxy bump, a flat, flesh-colored or brown scar-like lesion, a bleeding or scabbing sore that heals and returns
Basal cell carcinoma occurs most often on areas of the skin that are exposed to the sun, such as your head and neck. Most basal cell carcinomas are thought to be caused by long-term exposure to ultraviolet (UV) radiation from sunlight. Avoiding the sun and using sunscreen may help protect against basal cell carcinoma.


Causes:
Basal cell carcinoma occurs when one of the skin’s basal cells develops a mutation in its DNA. Basal cells are found at the bottom of the epidermis — the outermost layer of skin. Basal cells produce new skin cells. As new skin cells are produced, they push older cells toward the skin’s surface, where the old cells die and are sloughed off.
The process of creating new skin cells is controlled by a basal cell’s DNA. The DNA contains the instructions that tell a cell what to do. The mutation tells the basal cell to multiply rapidly and continue growing when it would normally die. Eventually, the accumulating abnormal cells may form a cancerous tumor — the lesion that appears on the skin.
Squamous cell carcinoma:
Squamous cell carcinoma is a type of skin cancer caused by an overproduction of squamous cells in your epidermis, the top layer of your skin. It is the second most common form of skin cancer after basal cell carcinoma. Most often, squamous cell carcinoma occurs on sun-exposed areas of your body, such as your face, ears and hands. People with darker skin are more likely to develop squamous cell carcinoma on areas that aren’t often exposed to the sun.


Squamous cell carcinoma may appear as:
- A firm, red nodule
- A flat lesion with a scaly, crusted surface
There are different types of squamous cell carcinoma based on where and how much cancer is in your body:
- Cutaneous: Cancer that only affects the top layer of your skin (in situ) or cancer that’s spread beyond the top layer of your skin.
- Metastatic: Cancer that’s spread to other parts of your body beyond your skin.
Causes:
A mutation to the p53 gene causes squamous cell carcinoma. The most common way that your p53 gene mutates is from ultraviolet (UV) exposure from the sun, or from using indoor tanning beds. The p53 gene provides instructions for your cells to divide and replicate to replace cells when they reach the end of their lifespan. Your p53 gene is a tumor suppressor, which means that the gene controls how much and how often your cells should create new cells. Too many cells create tumors, which can be cancerous.
A mutation to the p53 gene means that your cells don’t have the instructions they need to do their job correctly. As a result, your squamous cells divide and replicate too often, causing tumors (bumps, lumps or lesions) to form in and on your body.
Melanoma:
Melanoma is a kind of skin cancer that starts in the melanocytes. Melanocytes are cells that make the pigment that gives skin its color. The pigment is called melanin.
Melanoma can develop anywhere on your body, in otherwise normal skin or in an existing mole that becomes cancerous. Melanoma most often appears on the face or the trunk of affected men. Melanoma also can form in the eyes. Rarely, it can happen inside the body, such as in the nose or throat. In women, this type of cancer most often develops on the lower legs. In both men and women, melanoma can occur on skin that hasn’t been exposed to the sun.


The exact cause of all melanomas isn’t clear. Most melanomas are caused by exposure to ultraviolet light. Ultraviolet light, also called UV light, comes from sunlight or tanning lamps and beds. Limiting exposure to UV light can help reduce the risk of melanoma.
Melanoma signs include:
- A large brownish spot with darker speckles
- A mole that changes in color, size or feel or that bleeds
- A small lesion with an irregular border and portions that appear red, pink, white, blue or blue-black
- A painful lesion that itches or burns
- Dark lesions on your palms, soles, fingertips or toes, or on mucous membranes lining your mouth, nose, vagina or anus
Hidden melanomas
Melanomas also can develop in areas of the body that have little or no exposure to the sun. These areas may include the spaces between the toes and on the palms, soles, scalp or genitals. These are sometimes referred to as hidden melanomas because they occur in places most people wouldn’t think to check. When melanoma occurs in people with brown or Black skin, it’s more likely to occur in a hidden area.
Hidden melanomas include:
Melanoma inside the body: Mucosal melanoma develops in the mucous membrane. This tissue lines the nose, mouth, esophagus, anus, urinary tract and vagina. Mucosal melanomas are especially difficult to detect because they can easily be mistaken for other far more common conditions.

Melanoma in the eye:
Eye melanoma also is called ocular melanoma. It most often occurs in the layer of tissue beneath the white of the eye. This layer is called the uvea. An eye melanoma may cause vision changes and may be diagnosed during an eye exam.

Melanoma under a nail:
Acral-lentiginous melanoma is a rare form of melanoma that can occur under a fingernail or toenail. It also can be found on the palms of the hands or the soles of the feet. Acral-lentiginous melanoma tends to be very dark, flat and have very unusual borders. It’s more common in people of Asian descent and people with brown or Black skin.
Other, less common types of skin cancer include:
Kaposi sarcoma:

This rare form of skin cancer develops in the skin’s blood vessels and causes red or purple patches on the skin or mucous membranes. Kaposi sarcoma mainly occurs in people with weakened immune systems, such as people with AIDS, and in people taking medications that suppress their natural immunity, such as people who’ve undergone organ transplants.
Other people with an increased risk of Kaposi sarcoma include young men living in Africa or older men of Italian or Eastern European Jewish heritage.
Merkel cell carcinoma:

Merkel cell carcinoma causes firm, shiny nodules that occur on or just beneath the skin and in hair follicles. Merkel cell carcinoma is most often found on the head, neck and trunk.
Sebaceous gland carcinoma:
This uncommon and aggressive cancer originates in the oil glands in the skin. Sebaceous gland carcinomas — which usually appear as hard, painless nodules — can develop anywhere, but most occur on the eyelid, where they’re frequently mistaken for other eyelid problems.
Skin cancers are generally diagnosed clinically by a dermatologist or family doctor when learning of an enlarging, crusting, or bleeding lesion. The lesion will be inspected carefully, and ideally, a full skin examination will also be conducted.
Dermoscopy (using a special magnifying light) may be used to confirm the diagnosis, to detect early skin cancers, and to exclude benign lesions.
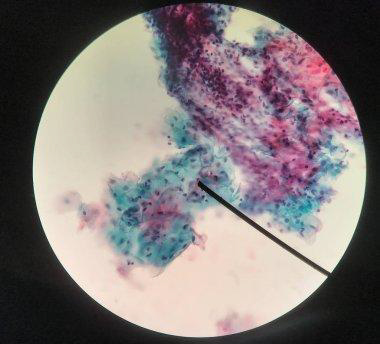
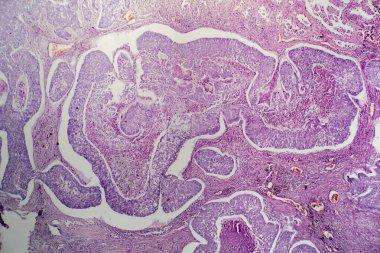
A partial skin biopsy may be taken in cases of suspected non-melanoma skin cancer to confirm the diagnosis or determine a subtype that may influence treatment.
Complete excision is usually undertaken to make a diagnosis if melanoma is suspected, as a partial biopsy can be misleading in melanocytic tumors.
The diagnosis is confirmed in the laboratory by a histopathologist. It can take a few days for the report to be issued, or longer if special tests are required.
Genetic testing for melanoma and blood-based melanoma detection may be available in some centers.
Further investigations may be required if there is a suspicion spread has occurred.
Treatment:
Early treatment of skin cancer usually cures it. The majority of skin cancers are treated surgically, using a local anesthetic to numb the skin. Surgical techniques include:
- Excision biopsy
- Wide local excision
- Mohs micrographic surgery
- Treatment options for superficial skin cancers include:
- Minor surgery including curettage and diathermy/cautery and electrosurgery
- Cryotherapy
- Topical therapy such as fluorouracil cream, imiquimod cream
- Photodynamic therapy (photosensitizing cream plus light)
- Radiotherapy (x-ray treatment)
- Lasers.
Treatment for advanced or metastatic basal cell carcinoma may include targeted therapies
Treatment for advanced and metastatic melanoma may include:
- Systemic immunotherapy using ipilimumab or checkpoint inhibitors pembrolizumab or nivolumab
- Topical and intralesional immunotherapy for melanoma metastases
- Targeted therapy against BRAF mutations using vemurafenib or dabrafenib or MEK inhibition with trametinib
- Combination medications, such as Cobimetinib
- Patients with skin cancer may be at increased risk of developing other skin cancers. They may be advised to:
- Practice careful sun protection, including the regular application of sunscreens
- Learn and practice self-skin examination
- Have regular skin checks
- Photographic surveillance
- Undergo digital dermoscopic surveillance (mole mapping), especially if they have many moles or atypical moles
- Seek medical attention if they notice any changing or enlarging skin lesions
- Take nicotinamide (vitamin B3) or acitretin (off-label) to reduce the number of squamous cell carcinomas.
These treatments can lead to adverse effects.
Most skin cancer can be completely cured with early treatment. Advanced skin cancers are more difficult to treat and can lead to death.


